Risk and severity
Cancer-affected patients are known to be at higher risk of severe COVID-19. Patients with haematological or lung malignancies, and the presence of metastatic disease are associated with a persistently increased risk, particularly in the first year of diagnosis and drops to baseline if diagnosed at later stages. For cancer at the metastatic stage, active disease confers significantly increased the risk of severe COVID-19. However, the data on the correlation between COVID-19 and cancer are lacking. The higher incidence, severity and mortality due to COVID-19 observed in patients with cancer as opposed to those without cancer remain observations based on non-comparative retrospective studies.
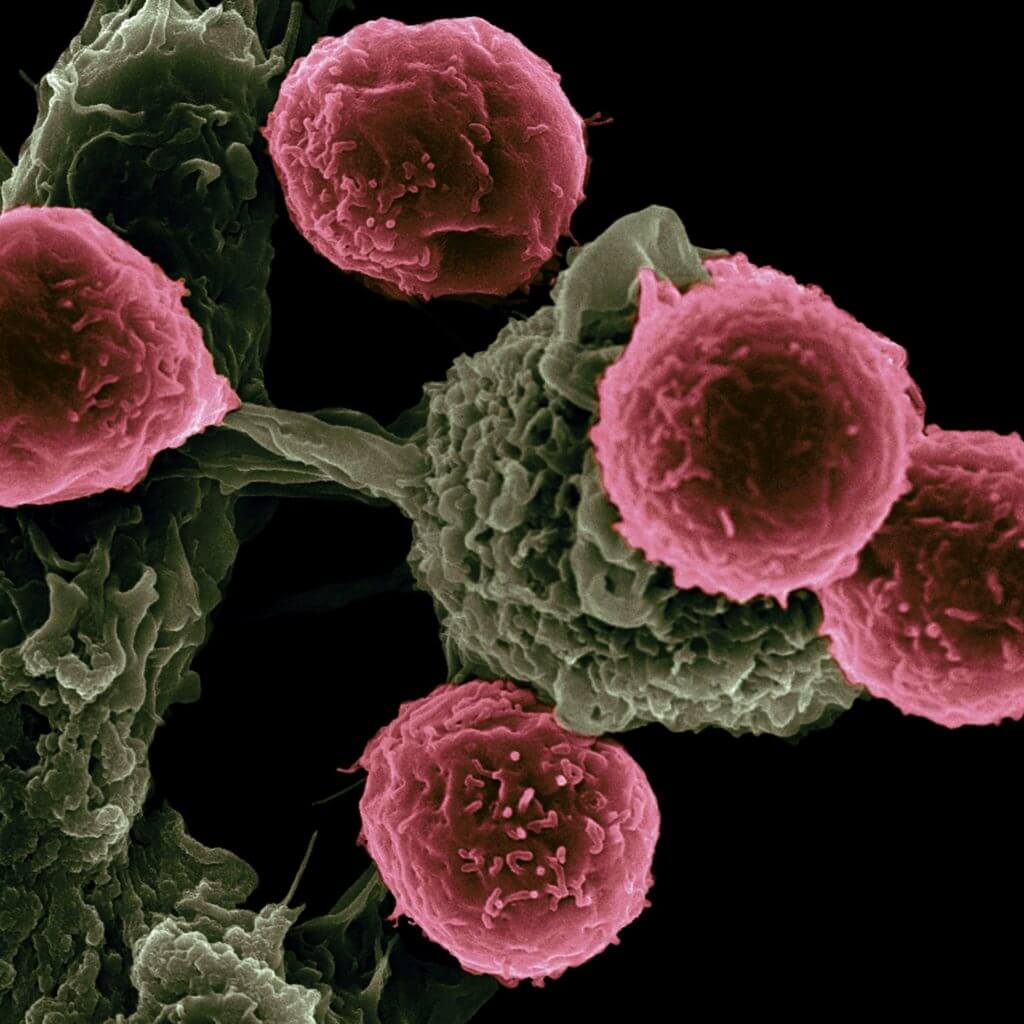
COVID-19 and Immune Checkpoints
A clinical study analysing the correlation between the expression of immune checkpoints and COVID-19 risk revealed that inhibitory expression of PD-1, A2A, BTLA, CD160, CD244, TIGIT, LAG3 and KLRG1, was increased in patients with mild symptoms while patients with severe symptoms or severely-affected patients had an expression of IDO1, CTLA4, CD276 and HAVCR2.
Stimulatory targets like ICOS, 4-1BB, CD27 and CD28 were elevated in mild patients in comparison to high and severe patients while expression of GITR (TNFRSF18) and CD40 were highest in severe patients.
It has also been observed that lung cancer patients treated with immune checkpoint inhibitors (ICI) had more severe COVID-19 infection. Whereas patients with other cancers who were treated with ICI demonstrated severe outcomes.
These data appear to support the usage of immune checkpoints as a biomarker for prognostic estimation of the severity of COVID-19, particularly in cancer patients.
Immune Checkpoint Inhibitors in COVID-19
In a retrospective analysis of 337 patients receiving anti-PD-1/PD-L1 for multiple solid tumors in Italy, only 0.9% (N=3), were hospitalised for COVID-19 without anyone being admitted to ICU. The authors claim that the data were inconclusive since the analysis did not consider the timing of initiation of therapy, there were no clear details on therapies given for COVID-19, no data on whether ICIs were given alone or in combination with another therapy were available, thus requiring further analysis.
There are numerous ongoing clinical trials listed on the clinicaltrials.gov investigating immune stimulation by targeting PD-1 (nivolumab, pembrolizumab and camrelizumab), rIL-2, IL-8, CSA0001 (LL-37 antiviral peptide with immunomodulatory functions), CD24FC (fusion protein that prevents TLR activation) and recombinant human granulocyte colony-stimulating factor (rhG-CSF). Other potential treatment strategies acting through indirect immune mediation that are currently under investigation are antiangiogenic agents bevacizumab (anti-VEGF), thalidomide (immunomodulatory) and ruxolitinib (JAK inhibitor).
Challenges with COVID-19 vaccination and cancer
The evidence of outcomes after COVID-19 vaccination in patients with cancer is limited. It is conceivable that the efficacy and safety of vaccination may be estimated to be similar to that of patients without cancer, although data from clinical trials are lacking. Hypothesizing based on the evidence of anti-infective vaccination in general (excluding live-attenuated vaccines and replication-competent vector vaccines) in patients with cancer, reduced vaccine-mediated protective effects may occur in patients treated with B cell-depleting agents (anti-CD19, anti-CD20, anti-CD10 monoclonal antibodies and CD19 CAR-T cells) due to a suboptimal immune response.
The level of efficacy is expected to be generally reduced in cancer patients with intense immunosuppression, such as recipients of HSCT or high-dose chemotherapy. It may also vary in patients with tumour type, cancer stage or therapy-induced immunosuppression.
The benefits of COVID-19 vaccination seem to significantly and substantially outweigh the risks. Given the immune-compromised status and the frailty of some cancer patients, dedicated clinical trials of COVID-19 vaccines in the oncology / haematology space are, therefore, required.
#oncology #haematology #cancer #covid19
Sources: